Abstract
Background: Cancer-associated thrombosis (CAT) is a common comorbidity in patients with cancer. Prior trials have demonstrated that direct oral anticoagulants (DOACs) and low-molecular weight heparins (LMWHs) are safe and effective for CAT management. Despite these data, treatment of CAT is complicated by consequences of both cancers and cancer-directed therapies that can impact anticoagulation options.
Methods: We developed the Northwestern Medicine CAT clinic in April 2020 to improve care by streamlining referrals for evaluation and management of CAT by a non-malignant hematologist. Patients were referred for either acute management of new VTE or for ongoing management of previously known VTE. Goal time-to-appointment for acute referrals was within 24 hours and for ongoing management within two weeks. Initial evaluations were completed by advanced practice providers with review by an attending classical hematologist and clinical pharmacist.
We manually reviewed electronic health records of patients seen in the CAT clinic since its inception. Data collected included demographic, cancer diagnosis and cancer-directed therapy, CAT clinic recommendations, and recurrent VTE, bleeding and death within 6 months of initial CAT clinic appointment. We used descriptive statistics to assess referral and treatment patterns.
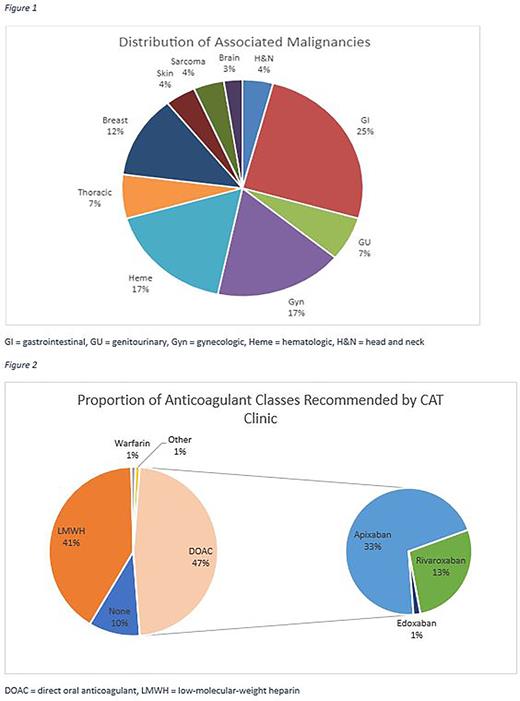
Results: One hundred twenty-two patients (N=122) were seen by CAT clinic clinicians between April 2020 - April 2022, including 63 (51%) in the first year. Patients had a median age of 63 years and 56.4% were female. Appointments occurred in nearly equal proportion via telehealth (50.8%) and in-office visits (49.2%) during these two years; however, 78% of visits were telehealth during the first year, and only 25.4% during the second. Forty-three (35.2%) referred for acute management were seen at a median time of two days, and the remainder for ongoing management were seen at a median time of 10 days. Referrals were predominantly for PE (25.4%), concurrent PE/DVT (23.0%), and proximal lower extremity DVT (18.9%); however, consults included thrombi of the cerebral, pulmonary, and splanchnic veins, as well as tumor thrombi, arterial thrombi, and need for primary prophylaxis. Tumor types were categorized into nine groups, with the largest proportion consisting of gastrointestinal (25.4%), gynecologic (17.2%), and hematologic (17.2%) malignancies (Figure 1).
DOACs were recommended in 47.5%, and LMWHs in 41% (Figure 2), with a similar proportion of DOACs prescribed between year one (47.5%) and year two (47.6%). Primary reasons for choosing LMWHs over DOACs were perceived bleeding risk (40%), tumor type (22%), and prior DOAC failure (20%). Twelve (9.8%) patients were advised to stop anticoagulation, due to lack of indication for 11 (91.7%) and perceived bleeding risk for one (8.3%). Four were referred for inferior vena cava (IVC) filter retrieval. At the time of evaluation, 16 (13.1%) patients were noted to have platelet counts <150,000/µL, but none had platelet counts <50,000/µL.
Within 6 months of initial evaluation, 11 (9.0%) patients developed progressive or recurrent VTE. Fourteen (11.5%) patients experienced bleeding: eight (57.1%) had major bleeding episodes as defined by the International Society on Thrombosis and Hemostasis, and six (42.9%) had clinically-relevant non-major bleeding. Among major bleeding events, six (75%) were gastrointestinal and two (25%) intraabdominal in origin, with no identified intracranial hemorrhages. Twenty (16.4%) died during the follow up period. Seventy-six (61.8%) patients were seen for a follow up visit after initial consultation.
Conclusion: Building the CAT clinic led to improved access to classical hematologists with thrombosis expertise to manage CAT. Historical wait times for this specialty have exceeded 90 days, while those referred to the CAT clinic had a median time-to-appointment of only nine days. Highlighting the complexity of CAT management, more than 40% of patients were not treated with DOAC, primarily related to perceived bleeding risk. Four patients were identified for IVC filter removal, suggesting there may be additional benefits to non-malignant hematologists beyond anticoagulant management. Decisions regarding treatment of individual patients with CAT remain complex, and access to thrombosis specialists provides additional expertise to optimize care.
Disclosures
Kalhagen:Harborside: Consultancy; Incyte Corporation: Speakers Bureau. Zakarija:Bayer: Other: Consultancy Advisory Board. Stein:Pharmassentia: Other: Advisory Board and Steering Committee. Martin:Janssen: Research Funding; Penumbra: Other: Scientific Advisory Board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal